Uveitis
What is it?
Uveitis is defined as unwanted inflammation in the eye. The inflammation can occur in the cornea or clear dome over the front of the eye (keratitis), white of the eye (scleritis), the front chamber of the eye (iritis), the front and middle chamber of the eye (iridocyclitis) only the middle chamber of the eye (intermediate uveitis), the back of the eye (posterior uveitis or retinitis), or in the entire eye (panuveitis). The reason for this unwanted inflammation can be infectious, such as parasites, bacteria, and viruses. Other causes of inflammation in the eye include diseases of the whole body, and genetic abnormalities. Sometimes the cause of the inflammation is indeterminant. Extensive laboratory testing and pictures of the eye and retina can help. Suppressing and stopping the inflammation is the main treatment goal. Numerous medications are used, including steroids and sometimes anti-cancer drugs. At Teton Retinal Institute, we have extensive experience and expertise with uveitis.
Symptoms of Uveitis (Eye Inflammation)
The symptoms of uveitis depend on where the inflammation is located (front, middle, back, or the entire eye):
- Redness and Pain: Common in the front of the eye (Iritis or Scleritis).
- Light Sensitivity (Photophobia): Discomfort when exposed to bright lights.
- Blurred Vision: Can occur if inflammation affects the cornea or the retina.
- Floaters: Small dark spots or "cobwebs" drifting in your field of vision (common in Intermediate or Posterior Uveitis).
- Sudden or Gradual Vision Loss: In severe cases, or if the entire eye is involved (Panuveitis).
Inherited retinal diseases or retinal dystrophies
What is it?
These genetic retinal abnormalities affect the back of the eye causing slow, unrelenting peripheral and central vision loss. Retinitis pigmentosa or RP is the most common genetic retinal disease. There are several different types of RP. Additionally, there are several other rarer retinal dystrophies. An evaluation by a retinal specialist, including specialized pictures of the retina, can identify your problem earlier and lead to genetic testing. The validity and methods of genetic testing have dramatically improved in the last 10 years. A few genetic treatments are available for RP. Lifestyle modifications also help. Teton Retinal Institute has diagnosed, tested, and managed many patients with genetic retinal diseases for more than 30 years.
Symptoms of Inherited Retinal Diseases (RP and Dystrophies)
Genetic conditions usually progress slowly over many years. Watch for:
- Night Blindness: Significant difficulty seeing in low light or at night.
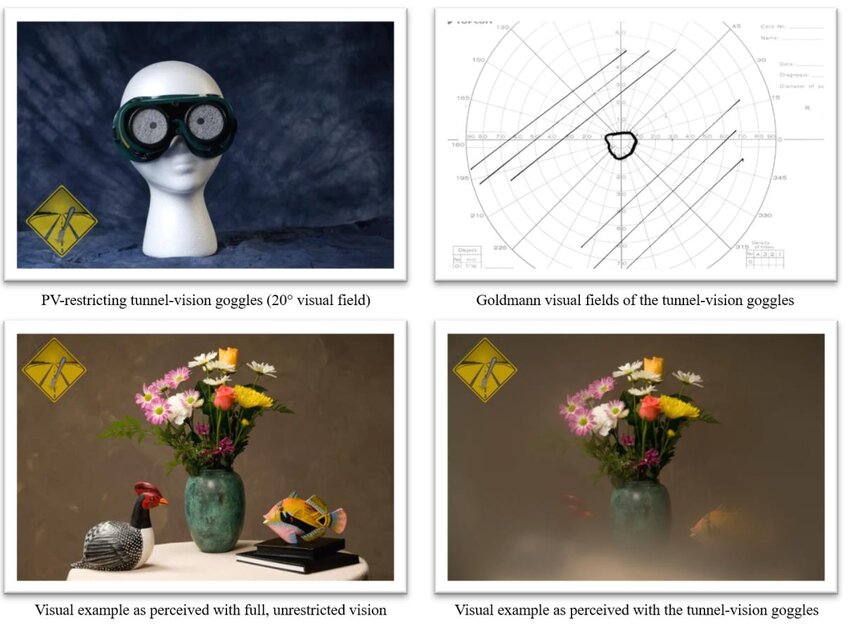
- Tunnel Vision: The gradual loss of side (peripheral) vision.
- Loss of Central Vision: Difficulty reading or recognizing faces as the disease affects the macula.
- Slow Recovery from Glare: Taking an unusually long time to adjust when moving from a bright environment to a dark one.
Frequently Asked Questions
-
If I have Uveitis, does it mean I have an underlying disease elsewhere in my body?
Not necessarily, but it is a possibility. Uveitis is often "idiopathic," meaning it occurs only in the eye without a clear outside cause. However, because the eye is connected to the rest of the body’s immune system, inflammation can be a sign of systemic conditions like sarcoidosis, lupus, or rheumatoid arthritis. This is why we often perform blood work and coordinate with your primary care doctor or a rheumatologist.
-
Why are "anti-cancer" drugs sometimes used to treat eye inflammation?
While the term can be intimidating, certain medications originally developed for oncology are highly effective at suppressing the overactive immune response that causes Uveitis. When steroids alone aren't enough—or if a patient needs to avoid long-term steroid side effects—these "immunomodulatory" drugs are used in much lower doses to safely "calm" the inflammation and protect the delicate tissues of the retina.
-
Can Uveitis come back after treatment?
Uveitis can be a "one-time" event (acute) or a recurring condition (chronic). Because it is an inflammatory response, it can flare up again if the underlying cause isn't fully managed or if the immune system is triggered. Regular follow-up appointments at Teton Retinal are essential to monitor for "quiet" inflammation that you might not even feel but could still damage your vision.
-
If I am diagnosed with an inherited retinal disease like RP, should my family members be tested?
Because these conditions are genetic (passed down through DNA), your results can provide important health information for your children, siblings, or parents. Genetic testing doesn't just help you; it can help your family members understand their own risks or identify if they are "carriers" of the gene. We can discuss the benefits of family screenings during your consultation.
-
What specific "lifestyle modifications" help with Retinitis Pigmentosa?
While we cannot change your genetics, we can help protect the remaining retinal cells. Common recommendations include:
- UV Protection: Wearing high-quality, wrap-around sunglasses to protect the retina from blue light and UV damage.
- Nutritional Support: Certain vitamins and antioxidants (such as Vitamin A Palmitate, Lutein, and Omega-3s) may be recommended depending on your specific type of dystrophy.
- Low Vision Tools: Utilizing specialized lighting, magnifiers, and digital aids to maximize your functional vision for daily tasks.

Don’t Wait — Protect Your Vision Now
Eye inflammation and retinal dystrophies require precise, expert intervention. If you are experiencing redness, pain, or changes in your peripheral vision, contact us immediately for a comprehensive evaluation by a retinal specialist.
Request an Appointment or call 208-535-4900 for immediate care at Teton Retinal Institute.
