
What Is Retinal Detachment? Symptoms, Causes, Risks and Treatments
This is a serious eye disease that can lead to blindness. At the first sign, act decisively and see a doctor immediately. The retina is a thin layer of tissue at the back of the eye. Retinal detachment occurs when the retina separates from the underlying structures that nourish and support it. We’ll discuss the main symptoms of retinal detachment, so you know what to do if something happens.
What is Retinal Detachment?
Globally, over 2 billion people live with vision impairment. Retinal detachment is extremely dangerous because it can lead to sudden and permanent vision loss. Let’s discuss this in more detail. The retina is responsible for perceiving light and transmitting visual signals to the brain. When it separates from the supporting tissues, the supply of oxygen and nutrients is disrupted, which is extremely dangerous. This situation causes rapid vision deterioration. If left untreated, it can lead to irreversible blindness. So don’t delay! See a specialist immediately.
Signs of Retinal Detachment
What symptoms should you be wary of?
- The sudden appearance of multiple “floaters” before your eyes;
- Flashes of light.
- A shadow or cloud in your field of vision.
- Even if there is no pain, symptoms may indicate the onset of retinal detachment. Be sure to take action.
Types of Retinal Detachment
There are two main types.
Rhegmatogenous Retinal detachment is the most common type. This occurs when a retinal tear allows the vitreous gel or humor to seep under the retina and lift it off the back of the eye. It is more common with age and after cataract surgery.
Traction retinal detachment develops when scar tissue on the surface of the retina pulls on it. The most common cause is diabetic retinopathy. People with diabetes should have regular checkups.
Retinal Detachment Causes
Researchers and retinal specialists have learned separation of the vitreous gel is an important precursor to developing retinal tears, and detachments. With age, the vitreous gel gradually liquefies, and contracts which usually leads to its safe separation from the retina and is benign. However, in a few individuals, the vitreous gel partially separates from the retina, but continues to pull in a few peripheral areas resulting in tears. Now the vitreous gel may seep through the tear, lifting the retina off the back of the eye.
Major risk factors are myopia (nearsightedness) and previous eye surgery, particularly cataract surgery. In people with myopia, the eyeball is elongated, leading to stretching and thinning of all the layers of the eye. In these stretched and peripheral areas, the retina becomes more fragile and prone to tears and degenerative changes, such as lattice degeneration, which is itself a serious risk factor.
Any eye or head injury (including contusions) can directly lead to a retinal tear or detachment. Certain eye surgeries can increase the risk of subsequent retinal detachment. Secondary retinal detachments caused by other diseases constitute a separate group of causes. A prime example is diabetic retinopathy. In this case, long-term elevated blood sugar damages the retinal blood vessels. This leads to the growth of abnormal blood vessels and the formation of scar tissue, which, when contracted, can pull the retina away from its underlying layers. Developmental abnormalities of the vitreous body and retina are associated with some hereditary eye diseases.
If a patient has already been diagnosed and treated for retinal detachment in one eye, this is a significant risk factor for developing a similar condition in the fellow eye.
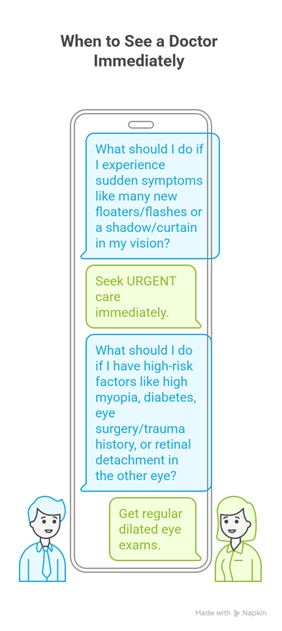
When to See a Doctor Immediately
| Signs & Risk Factors | Action |
|---|---|
Sudden Symptoms:
|
Seek URGENT care |
High-Risk Factors:
|
Get regular dilated eye exams |
Diagnosis
Take care of your vision and have regular eye exams. A specialist diagnoses retinal detachment using the following tests:
- Visual acuity testing,
- peripheral vision testing,
- intraocular pressure measurement;
- fundus examination using indirect ophthalmoscopy;
- Ultrasound examination of the eye. This test is especially important in cases of corneal, lens, or vitreous opacities, when the retina cannot be seen. The doctor first dilates the pupil with special drops. Ultrasound is a safe, non-invasive examination of the internal structures of the eye. The procedure helps assess the condition of the crystalline lens, vitreous body, retina, and optic nerve.
- Optical coherence tomography produces layer-by-layer “photo slices” of the retina with microscopic resolution.
- Fundus photography creates detailed portraits of the fundus. These images are an invaluable diagnostic tool.
- Computer tomography (CT) and MRI scans are only used rarely to diagnose retinal detachments. This method allows high-resolution differentiation of biological tissues based on their radiographic density. It is a radiographic method for layer-by-layer examination of the structures of the eye and orbit, based on obtaining multiple tissue cross-sections followed by computer reconstruction of the images in three projections. Doctors use orbital CT scans to visualize the structures of the eyeball and the bony walls of the orbit when retinal detachment is suspected. Your doctor will be able to determine which method is appropriate for your specific case.
Treatment of retinal tears, and detachments
The most common form of retinal detachment starts with a retinal tear. As such, early patient presentation and early detection of retinal tears without a detachment can be successfully treated with laser or freezing surgery in the doctor’s office. However, a retinal tear with a detachment is a more complex problems usually requiring surgery in the hospital.
Retinal Detachment in Diabetes or Tractional Retinal Detachments
For patients with diabetes early detection and frequent monitoring are paramount. Earlier treatment with specialized eye injections, and laser surgery has dramatically improved visual results. More severe cases of diabetic retinopathy with scar tissue may require vitrectomy in the hospital. However, many patients are helped. Today, no person with diabetes should ever go blind unless they delay seeing an eye surgeon.
Hospital based surgery, Post-operative Care and Complications
Postoperative care is individualized. Your eye surgeon will use prescription eye drops and may have special face down or side down positioning requirements after hospital base surgery. Compliance with postoperative instructions is essential to better outcomes.
Office-based Retinal Surgeries are Less Complex and Have Less Postoperative Requirements
Sometimes, despite the doctor and patient doing everything right, complications occur. Your eye surgeon will carefully monitor you for complications. If they arise, you may need more office based or hospital based surgery, more prescription medications, or a longer time to heal. Do not become discouraged, but continue to persevere. The patient’s continued compliance and perseverance will result in a better outcome.
Factors Determining Treatment Success
The prognosis for visual recovery is highly individualized. It directly correlates with two key factors: the extent of the detachment and the duration of the pathology before surgical correction. The earlier the intervention is performed, the higher the chances of success.
Modern vitreoretinal techniques allow for stable anatomical reattachment of the retina in the vast majority of cases. Vision recovery is gradual and may be incomplete, especially if the macular region is involved. Sometimes, the specialist recommends repeat surgeries.
Prevention of Retinal Detachment: Vision Preservation Strategies
Enter regular ophthalmological examinations. Regular dilated fundus monitoring is essential for individuals with high myopia, diabetic retinopathy, and a strong family history. Wearing protective eyewear when playing contact sports, working with tools, and in high-risk environments can help prevent direct damage.
Achieve target blood glucose levels if you have diabetes and stabilize your blood pressure. This significantly reduces the risk of secondary retinal damage. Seek prompt medical attention. The appearance of photopsia (flashes of light) or a sudden increase in the number of “floaters” or “films” before the eye requires immediate consultation with an ophthalmologist.
Life after Surgery
The success of surgical treatment directly depends on the patient’s adherence to all recommendations during the postoperative period. Strictly follow your doctor’s instructions. Use the prescribed eye drops regularly (antibacterial, anti-inflammatory). Temporarily limit physical activity, especially those involving heavy lifting, bending, and vibration. Maintain the prescribed head position (face down or sideways) while sleeping for the period recommended by your doctor. Increasing pain, hyperemia, swelling, discharge from the eye, or, especially, sudden deterioration of vision are absolute indications for immediate emergency ophthalmological care.
Conclusions
Don’t delay your visit to the ophthalmologist/eye MD or preferably a retinal specialist. Your vision can be saved with timely intervention. Early detection and intervention are crucial!



